Respiratory health disparities in the United States and their economic repercussions

Chronic respiratory diseases such as asthma, lung diseases, and pulmonary hypertension are now the third-leading cause of death in the United States, killing more than 150,000 people a year. While the overall cardiovascular mortality rate has dropped sharply over the past 50 years, a large portion of the population has not experienced this decline. A recent research paper shows the uneven prevalence of chronic diseases and exposure to risk factors among demographic groups defined by race, ethnicity, and socioeconomic status.1 The prevalence of asthma is sharply higher among the poor and in African American communities. (See Figure 1.)
Figure 1

Respiratory diseases intensify economic inequality through the cyclical nature of disparate health outcomes. Disadvantaged groups end up living in areas more exposed to risk factors. These groups develop respiratory problems that prevent them from going to work, and they struggle to improve their economic situation. This issue brief contextualizes the relationship between respiratory health problems and how structural inequities such as environmental segregation and residential racism play a role in the persistence of economic inequality.
How does respiratory disease impact economic growth?
The inflexible work culture in the United States contributes to the financial strain of adequately providing care for families while maintaining stable employment. Sickly people and primary caregivers experience job insecurity by not having paid leave and flexible work schedules. Connecting social inequities with health inequities provides insight on how people are locked out of obtaining and building wealth.
Indeed, having a chronic disease impacts working conditions and worker productivity significantly, slowing down economic growth. Estimates indicate that Chronic Obstructive Pulmonary Disease, or COPD, and asthma cost U.S. society between $50 billion2 and $56 billion3 a year, respectively. Professors Thomas LaVeist of John Hopkins University, Darrell Gaskin of the University of Maryland, and Patrick Richard of George Washington University, focusing on the years 2003 to 2006, estimated that eliminating health disparities would have considerably decreased medical expenditures by $229 billion during this period.4
University of California, San Francisco professors Mark Eisner, Edward Yelin, Laura Trupin, and Paul Blanc demonstrated a strong relationship between chronic respiratory diseases and work disability in their 2002 study, “The Influence of Chronic Respiratory Conditions on Health Status and Work Disability.”5 The co-authors used the California Work and Health Survey to interview workers about their health conditions and observed that employees with asthma, COPD, or other breathing disorders perceived “a limitation in the amount of work they could perform.” Additionally, among COPD-infected adults, the likelihood of current employment was lower than for people with no chronic diseases. These costs are a significant drag on the economy. Sarah Barnett and Tursynbek Nurmagambetov of the Centers for Disease Control and Prevention estimate that the economic costs of asthma in 2007 resulting from missed workdays were $3 billion.6
Families with small children are hit the hardest, according to the authors of “State-level medical and absenteeism cost of asthma in the United States.”7 Children aged 0 to 17 years old with major respiratory health concerns miss an average of 2.2 days of school upon entering primary and secondary education, and fall behind their peers who do not miss school due to asthma-related issues. And parents suffer work-related concerns. The authors find that parents who take parental leave if offered by their employers lose an estimated total average of $1.19 billion. Single-parent homes are especially hard hit if forced to miss work to take care of children.
Even more striking is this survey conducted by the University of Michigan: Roughly one-third of parents claim that taking days off in order to take care of their sick child could lead to them losing pay or losing their job.8 These economic outcomes unevenly harm African Americans, Hispanic migrants, and lesbian, gay, bisexual, and transgender Americans. Below, we discuss the unique challenges facing each of these populations.
African Americans
Black children uniquely experience environmental harm because they live in neighborhoods that are oftentimes too close in proximity to chemical waste fields and factories. Federal Reserve economist Diana Alexander and Janet Currie of Princeton University sought to explain the disparity of asthma rates between black children and nonblack children.9 They examined the relationship between asthma, race, birth weight, and location. Using data on health outcomes and geographic location of children in New Jersey, they found key environmental differences between black and nonblack ZIP codes that determine the prevalence of asthma among children with low birth weights.
Because of the neighborhoods they live in, black children are more likely to experience structural racism—social and institutional factors that contribute to racial inequality. These social structures and economic systems include the social environment, physical environment, health services (or lack thereof), residential segregation, inadequate enforcement of housing policies, and lack of access to economic opportunities. African Americans are much more likely to be uninsured relative to whites and those with higher incomes. Low-income individuals and people of color face increased barriers to accessing care, receive poorer quality care, and ultimately experience worse health outcomes.
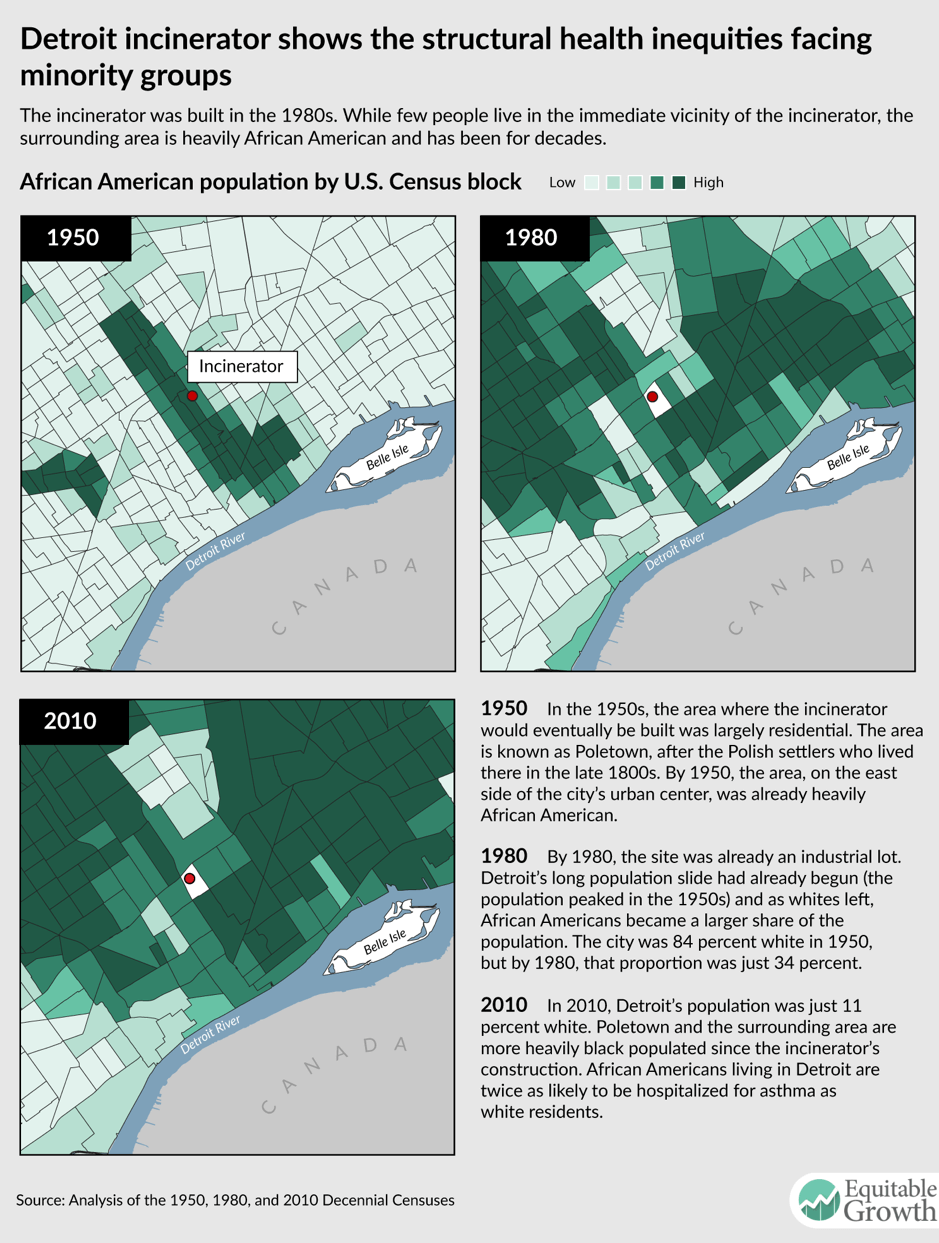
In Detroit, for example, the average family income is $25,764; the residents are 82 percent black; and there is the world’s largest municipal incinerator. The toxins emitted by the incinerator have been shown to be hazardous to human health and particularly children in their formative stages.10 The connection between the location of the incinerator, built in the mid-1980s, and the racial composition of Detroit neighborhoods over the past three decades is telling. (See Figure 2.)
Figure 2
The placement of polluting industries near low-income and majority-black neighborhoods is a pattern repeated across the country. Outcomes for health in New York City, for example, also demonstrate the drastic difference of living in black ZIP codes as opposed to white neighborhoods. The Dyker Heights and Bay Ridge communities are both 60 percent white and experienced just 94 avoidable adult-asthma hospitalizations per 100,000 residents. In contrast, residents in Bedford-Stuyvesant in Brooklyn—where the population is 64 percent black—experienced a rate almost 6 times as high: 531 avoidable adult-asthma hospitalizations per 10,000 residents.11 To make matters worse, in this community, one in five adults had no health insurance, and one in eight went without needed medical care prior to 2014 (implementation of the Affordable Care Act has reduced these rates in New York City generally and should also reduce rates in these neighborhoods). The residents in this neighborhood experience the poorest housing conditions due to housing-related exposures to cockroaches, mice, and lead. In fact, Bedford-Stuyvesant is affected by the most harmful air pollutants in New York City.
Studies of Baltimore also demonstrate the impact of ZIP code on respiratory disorders.12 Residents in ZIP code 21223 visit hospitals for asthma at 4 times the rate of other, wealthier areas. Ironically, prestigious medical centers—Johns Hopkins and the University of Maryland Medical Center—are located close to this neighborhood and receive substantial tax breaks for providing “community benefits.” These health institutions’ lack of attention is likely to increase the cost of this issue; as explained by Ben Carson, currently the secretary of the U.S. Department of Housing and Urban Development and previously a surgeon at Johns Hopkins, “the cost of not taking care of people is probably greater than the cost of taking care of them.”13
Hispanic migrants
Asthma is a complex sickness due to both genetic and environmental factors, which lead to increased prevalence of the disease among migrants. As explained by University of Pittsburgh’s Fernando Holguin and Mark Schenker of the University of California, Davis, migrants who move from less-industrialized countries to more-developed ones face increased prevalence of asthma over time.14 They discuss two main reasons for this phenomenon: acculturation and occupational hazard. Additionally, Wake Forest University professors Ann Hiott, Joseph Grzywacz, Stephen Davis, Sara Quandt, and Thomas Arcury found that in 2008, the combination of stress, depression, or anxiety with environmental factors led to a higher risk of developing chronic respiratory diseases for migrant farm workers.15
Then there are the health problems associated with acculturation, the process by which migrants change their attitudes toward those of the host society.16 This phenomenon seems to affect the prevelance of respiratory diseases, especially for the Hispanic population. Although Hispanics of Mexican descent have a lower prevalence of asthma (5.3 percent) than the rest of the American population (7.6 percent),17 the risk of having asthma among Mexicans that have migrated to the United States is less than half the risk facing Mexicans born in the United States.18
A study of Canadian migrants examined what the reserachers call the “healthy immigrant effect.” They find that the risk of having a disease for more acculturated families approaches the one of the host country. Elizabeth McQuaid of Brown University and Daphne Mitchell and Glorisa Canino of the University of Puerto Rico explain that acculturation leads to migrants having contact with new types of allergens, an increased smoking rate compared to Mexico, and higher rates of obesity.19 Spanish-speaking parents are also less likely to be taught what to do during asthma attacks or to have access to health insurance.
Fernando Holguin of the University of Pittsburgh and Marc Schenker of the University of California, Davis focus on the incidence of working conditions and occupational hazard among Hispanic migrants.20 According to the NAWS 2009–2010 Survey, 82 percent of the 5 million people hired as farm workers are Hispanic. Since nearly half of them are not legally authorized to work in the United States, they have limited access to health benefits. Moreover, farming work increases the risk of asthma because workers are exposed to pesticides and dust, and live in low-quality housing with poor ventilation and mold. No wonder researchers documented rates of depression as high 30 percent to 46 percent for migrant workers,21 mainly explained by their isolation from the rest of the society due to cultural and language barriers.
Lesbian, gay, bisexual, and transgender Americans
More than 10 million Americans self-identify as LGBT, but the respiratory disparities linked to sexual orientation remain understudied. John Blosnich, Joseph Lee, Robert Bossarte, and Vincent Silenzio of the University of Rochester examined the 2004 Behavioral Risk Factor Surveillance System and found a significantly higher rate of asthma among same-sex partners.22 In the sample studied, the prevalence of asthma among same-sex male couples was 12.3 percent, compared to just 5.9 percent for heterosexual men. This pattern was even more pronounced among women: 21.4 percent for same-sex partners, versus 9.5 percent for heterosexual ones.
Emily Clausen of Duke University and Alison Morris of the University of Pitsburgh suggest two factors to explain the higher prevalence of respiratory disease among LGBT Americans.23 First, they are less likely to see a physician for fear of disapproval. They experience a “perceived pressure to hide sexual orientation” that does not affect other populations. A 2010 study quantifies this pressure.24 It found that only 60 percent of bisexual and homosexual women get a routine annual checkup, compared to 71 percent of heterosexual women. Moreover, physicians are not always trained to deal with LGBT health-related issues: One-third of medical education programs do not include this theme.25
Second, cigarette and alcohol use is more prevalent in the LGBT community. A review of the available data in 2009 highlighted the higher prevalence of smoking in the LGBT population.26 The data show that 23.9 percent of LGBT adults smoke cigarettes, compared to just 16.6 percent of straight adults.27 In addition, the rate of binge drinking among lesbian and bisexual women is roughly twice that of heterosexual ones.28
How can respiratory health equality be achieved?
Respiratory inequalities are an ethical issue but also are an important component of equitable economic growth. Some groups are held back economically because of where they are born or where they live due to health-related disparities. Comprehensive policies to protect these vulnerable populations should address this issue by promoting health reform that targets specific populations. Prevention campaigns targeting minorities, promotion of ethnic diversity among medical school students, and an increase in Medicaid coverage for medical fees associated with respiratory diseases are among the policies that could be pursued to address these health inequities and break the cycle of economic deprivation caused by respiratory diseases.
—Dionna Cheatham previously worked at the Washington Center for Equitable Growth and is now a BSC Consultant for the Office of Planning, Research and Evaluation at the U.S. Department of Health and Human Services. Iris Marechal was an intern at the Washington Center for Equitable Growth in 2017–2018 and is now pursuing a double master’s degree in corporate and public management at HEC and SciencesPo Paris.
End Notes
1. Juan Carlos Celedón, ed., Achieving Respiratory Health Equality, A United States Perspective (New York, NY: Humana Press, 2017).
2. Amir Qaseem and others, “Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society,” Annals of Internal Medicine 155 (3) (2011): 179–191, available at https://www.ncbi.nlm.nih.gov/pubmed/21810710.
3. Sarah Beth Barnett and Tursynbek Nurmagambetov, “Costs of asthma in the United States: 2002-2007,” The Journal of Allergy and Clinical Immunology 127 (1) (2011): 145–152, available at https://www.ncbi.nlm.nih.gov/pubmed/21211649.
4. Thomas LaVeist, Darrell Gaskin, and Patrick Richard, “Estimating the economic burden of racial health inequalities in the United States,” International Journal of Health Services 41 (2) (2011): 231–238, available at https://www.ncbi.nlm.nih.gov/pubmed/21563622.
5. Mark D. Eisner and others, “The Influence of Chronic Respiratory Conditions on Health Status and Work Disability,” American Journal of Public Health 92 (9) (2002): 1506–1513, available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1447269/.
6. Barnett and Nurmagambetov, “Costs of asthma in the United States : 2002-2007.”
7. Tursynbek Nurmagambetov and others, “State-level medical and absenteeism cost of asthma in the United States,” Journal of Asthma 54 (4) (2017): 357–370, available at https://www.ncbi.nlm.nih.gov/pubmed/27715355.
8. C.S. Mott Children’s Hospital at the University of Michigan, “Sick kids, struggling parents” (2012), available at https://mottpoll.org/reports-surveys/sick-kids-struggling-parents.
9. Diane Alexander and Janet Currie, “Is it who you are or where you live? Residential segregation and racial gaps in childhood Asthma.” Working Paper 23622 (National Bureau of Economic Research, 2017), available at http://www.nber.org/papers/w23622.
10. United States Environmental Protection Agency, Children’s Environmental Health Disparities: Black and African American Children and Asthma (2014), available at https://www.epa.gov/sites/production/files/2014-05/documents/hd_aa_asthma.pdf.
11. New York City Health, Community health profiles 2015, Brooklyn Community District 3: Bedford Stuyvesant (2015), available at https://www1.nyc.gov/assets/doh/downloads/pdf/data/2015chp-bk3.pdf.
12. Julz Harvey, “In Southwest neighborhoods, more people are taking ambulances for asthma related emergencies,” Capital News Service, 2016, available at http://cnsmaryland.org/interactives/fall-2016/dec/asthma-baltimore/ambulance-asthma/index.html.
13. Jay Hancock, Rachel Bluth, and Daniel Trielli, “Hospitals find asthma hot spots more profitable to neglect than fix,” The Washington Post, December 4, 2017, available at https://www.washingtonpost.com/national/health-science/hospitals-find-asthma-hot-spots-more-profitable-to-neglect-than-fix/2017/12/01/0d804ce2-b806-11e7-be94-fabb0f1e9ffb_story.html?utm_term=.2f2c298b58dc.
14. Fernando Holguin and Marc B. Schenker, “Migrant Health.” In Juan Carlos Celedón, ed., Achieving Respiratory Health Equality (New York, NY: Humana Press, 2017).
15. Ann E. Hiott and others, “Migrant Farmworker Stress: Mental Health Implications,” The Journal of Rural Health 24 (1) (2008): 32–29, available at https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1748-0361.2008.00134.x.
16. Carolyn Williams and John Berry, “Primary prevention of acculturative stress among refugees. Application of psychological theory and practice,” The American Psychologist 46 (6) (1991): 632–641, available at https://www.ncbi.nlm.nih.gov/pubmed/1952422.
17. Centers for Disease Control and Prevention, “Most Recent Asthma Data,” available at https://www.cdc.gov/asthma/most_recent_data.htm (last accessed July 2018).
18. Fernando Holguin and others, “Country of Birth as a Risk Factor for Asthma among Mexican Americains,” American Journal of Respiratory and Critical Care Medicine 171 (2) (2005), available at http://www.atsjournals.org/doi/abs/10.1164/rccm.200402-143OC.
19. Elizabeth McQuaid, Daphne Koinis-Mitchell, and Glorisa Canino, “Acculturation.” In Juan Carlos Celedón, ed., Achieving Respiratory Health Equality (New York, NY: Humana Press, 2017).
20. Holguin and Schenker, “Migrant Health.”
21. Athena Ramos and others, “Stress Factors Contributing to Depression Among Latino Migrant Farmworkers in Nebraska,” Journal of Immigrant and Minority Health 17 (6) (2015): 1627–1634, available at https://www.ncbi.nlm.nih.gov/pubmed/25840517.
22. John Blosnich and others, “Asthma Disparities and Within-Group Differences in a National, Probability Sample of Same-Sex Partnered Adults,” American Journal of Public Health 103 (9) (2013): e83–e87, available at https://www.ncbi.nlm.nih.gov/pubmed/23865655.
23. Emily Clausen and Alison Morris, “The Lesbian, Gay, Bisexual, and Transgender Community and Respiratory Health.” In Juan Carlos Celedón, ed., Achieving Respiratory Health Equality (New York, NY: Humana Press, 2017).
24. John Blosnich and others, “Health Inequalities Among Sexual Minority Adults: Evidence From Ten U.S. states,” American Journal of Preventive Medicine 46 (4) (2014): 337–349, available at https://www.ncbi.nlm.nih.gov/pubmed/24650836.
25. Juno Obedin-Maliver and others, “Lesbian, Gay, Bisexual, and Transgender-Related Content in Undergraduate Medical Education,” JAMA 306 (9) (2011): 971–977, available at https://www.ncbi.nlm.nih.gov/pubmed/21900137.
26. J.G. Lee, G.K. Griffin, and C.L. Melvin, “Tobacco Use Among Sexual Minorities in the USA, 1987 to May 2007: a systematic review,” Tobacco Control 18 (4) (2009): 275–282, available at https://www.ncbi.nlm.nih.gov/pubmed/19208668.
27. Centers for Disease Control and Prevention, “Lesbian, Gay, Bisexual, and Transgender Persons and Tobacco Use,” available at https://www.cdc.gov/tobacco/disparities/lgbt/index.htm (last accessed July 2018).
28. John Blosnich and others, “Health Inequalities Among Sexual Minority Adults: Evidence From Ten U.S. states.”