Overview
Until recently, the policy debate over paid leave in the United States has most often focused on the need to expand access to paid parental and family caregiving benefits. Access to these benefits is lower in the United States than many other developed countries, and as women’s participation in the U.S. labor force grows, so too does the need for benefits to help workers juggle the competing demands of work and caregiving. Meanwhile, paid time off to address one’s own medical condition is the most frequently used type of paid leave, yet interestingly, has received far less attention in the policy debate and research.
The recent outbreak of COVID-19, the name of the disease spread by the new coronavirus, and the recession caused by policymakers’ failure to respond in a timely way to a growing public health crisis, has sensitized the country to the need for paid leave, especially paid sick leave. In response, Congress passed legislation that would provide some workers with temporary paid sick leave and caregiving leave.
Prior to the coronavirus pandemic, the lack of attention paid to medical leave was partly because more workers in the United States have access to it than the other types of leave. Approximately 42 percent of all U.S. private-sector employees had access to paid medical leave in the form of private short-term disability insurance in 2019, and 71 percent of workers had access to paid sick leave.1 Most workers who have access to short-term disability insurance have access through voluntary employer-provided plans. In addition, workers in six states now have access to paid medical leave through state-based programs, with three more plus the District of Columbia scheduled to begin paying benefits over the next 3 years.2
California, New Jersey, New York, and Rhode Island operate the oldest paid medical leave programs, known as temporary disability insurance programs.3 These programs offer benefits ranging from 26 weeks to 52 weeks. More recently enacted state medical leave programs are generally shorter in duration, offering benefits from 2 weeks in the District of Columbia to 20 weeks in Massachusetts (scheduled to begin in 2021). In addition, many state and local governments have enacted mandates on employers to provide paid sick leave.4
Still, access to these benefits is uneven and substantial unmet need exists, particularly for the country’s most vulnerable workers. Overall, access to paid medical leave through short-term disability insurance is higher among workers with higher incomes (63 percent in the top quartile), those working full time (51 percent), and in management, professional, and related occupations (58 percent).5 Gender and racial disparities also exist. In addition, according to the American Time Use Survey, a nationally representative survey of individuals, approximately 8.7 percent of workers reported not being able to take the leave that they needed (whether paid or unpaid) and that of this group, the most common reason for needing to take leave was to address their own medical condition (35.8 percent).6
As policy interest in expanding paid leave to address workers’ needs is growing, so too is interest in research to better understand paid medical leave and its potential impact on economic and health outcomes, its implications for employers, and paid leave’s interactions with other government programs and costs. To date, not much research has been done in the United States to directly assess the impact of paid medical leave on key outcomes. There is relatively more evidence from Europe and other developed countries, particularly around paid sick leave, that suggests paid medical leave is a worthwhile investment.
This research from other countries is important, but key social, economic, and programmatic differences make it difficult to translate those findings into specific recommendations for U.S. policy. Yet research in areas related to paid medical leave that looks at the intersection of health, disability, income security, and work provide important insights for understanding the impact of paid medical leave policies.
In this report, we aim to inform future research by first providing background on what paid medical leave is and highlighting important features that make it distinct from parental and family caregiving. We then describe what is known about the expected impact of paid medical leave and the ways in which it could be expected to affect economic and health outcomes, including effects on individuals, public health, employers, and the U.S. economy. We then describe key remaining questions and data sources that could be used for future inquiry.
The coronavirus pandemic and new policies enacted at the federal, state, and local level in response to this public health crisis and subsequent recession also are opening up new lines of inquiry. Workers are taking both short-term sick leave and longer medical leave because of the coronavirus. A better understanding of the overall research on sick and medical leave can help inform how we respond to this immediate crisis, as well as to future crises and the overall future health and well-being of workers and their families in the U.S. economy.
What is paid medical leave?
Paid medical leave is a benefit that allows an individual to take time off from work with pay to address their own serious medical condition that limits their ability to work. The term “medical leave” is generally used to refer to leave that lasts weeks or months. A condition that might require medical leave, for example, is cancer, which may require individuals to take time off from work for treatment, surgery, and recovery. Leave may be taken all at once, intermittently, or both.
The primary distinction between medical leave, sick leave, and long-term disability leave is duration. Sick leave, or paid sick days, is the shortest in duration, usually measured in days or occasionally up to several weeks. Sick leave is typically used for medical appointments and to address illnesses such as the common cold or flu. Medical leave is longer in duration than sick leave, lasting weeks or months, generally tapped to recover from serious illnesses or injuries. Long-term disability is for illnesses or injuries requiring months or years of recovery or a departure from the workforce. (See Table 1 for a breakdown of these various types of paid leave.)
Table 1
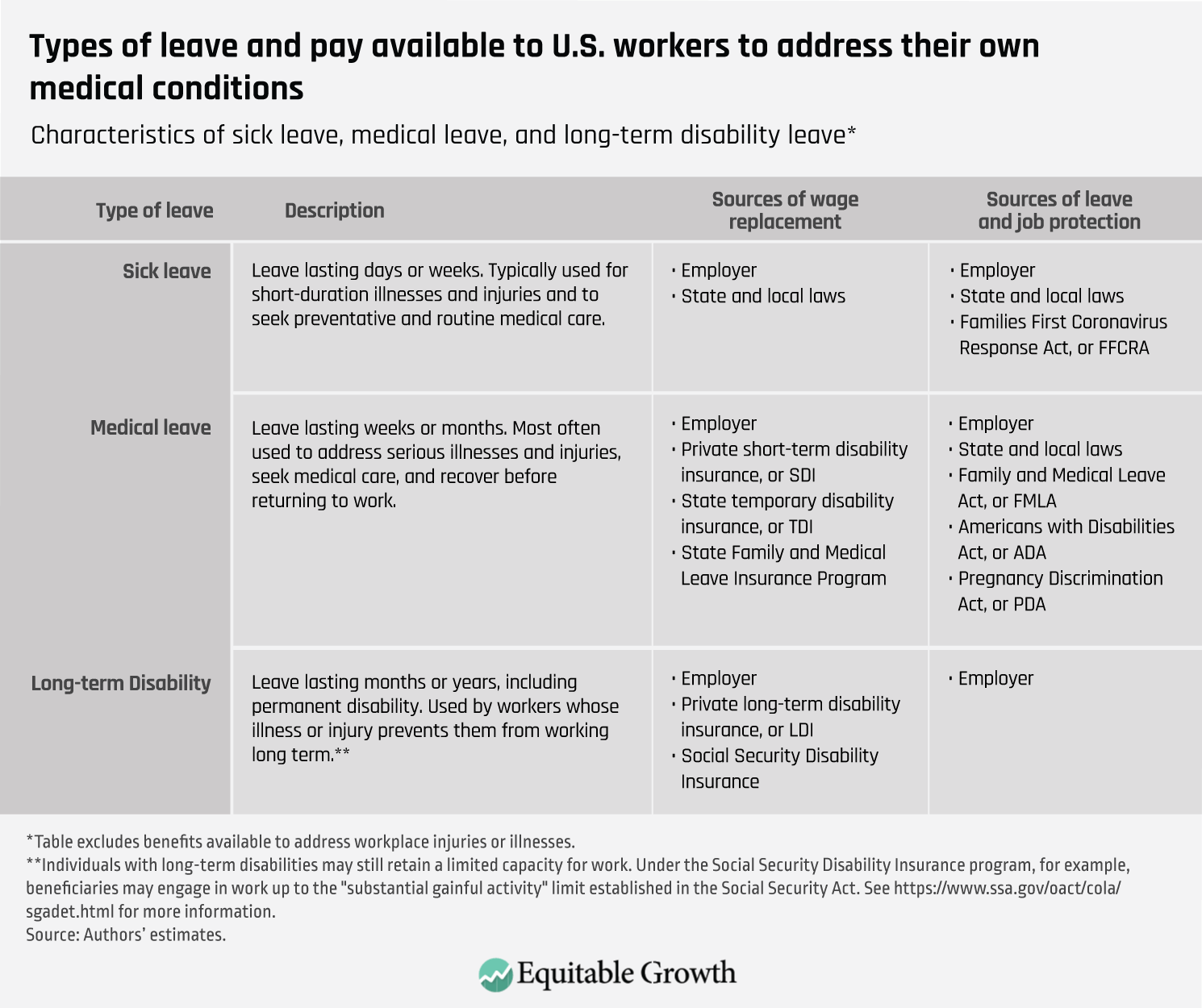
The differences between medical leave and long-term disability, however, are about more than the length of leave. Long-term disability refers to leave taken for months or years and where the individual is no longer able to work, either permanently or for a significant period of time, due to their condition, resulting in individuals on leave for long-term disability not being considered part of the labor force, though some may be. In contrast, individuals who take sick days or medical leave expect to return to work and so are still considered part of the labor force. A worker who injures their knee and requires surgery and time to recover, for example, may use paid medical leave to address their condition before transitioning back to work.
Medical leave may be paid or unpaid and may or may not be “job protected,” meaning workers have a right to retain their jobs or a similar one when they return from leave. Paid medical leave replaces either a share or all of workers’ wages while they are on leave. Whether workers receive pay while on leave depends on their employer’s benefits package and whether they live in a state with a public paid medical leave program. There is currently no federal paid medical leave benefit for workers to address their own serious medical condition that is not work-related.7
Whether a worker has a right to job-protected leave depends on whether they are a covered worker for the purposes of the federal Family and Medical Leave Act of 1993, as well as any other applicable federal, state, or local laws. The legal framework around leave-taking is layered and may consist of six or more distinct rights.8 Employers also may choose to provide access to unpaid leave for workers. Workers who have paid medical leave are also more likely to have job protection, but many workers do not have access to either of these benefits and rights.
Medical leave can be described as distinct from sick leave and long-term disability, but the reality for researchers and policymakers who want to understand the impact of policy on the outcomes of paid medical leave is that these distinctions are not always clear or consistently used. Major representative surveys on leave usage, for example, do not always distinguish between when a respondent is taking sick leave, medical leave, or short-term disability.
In addition, the term “sick leave” is used to refer to both sick leave and medical leave in many countries outside the United States, including European countries where medical leave is more widely available and where an important body of research exists. The ambiguity in terminology can create challenges for isolating the impact of medical leave from the other types of leave.
Context for understanding paid medical leave policy
Medical leave is distinct from parental and family caregiving leave in several ways that have important implications for research and policy. In this section we highlight important considerations for designing research studies and policies around workers’ needs to take leave to address their own health. This includes understanding that the condition underlying a medical leave claim is often itself a threat to the worker’s own health and economic security, and more workers take leave to address their own health than for any other reason.
In addition, a private market for this benefit already exists. Many workers with access to employer-paid benefits also receive additional help to return to work if they encounter hurdles. Last, special rights and protections exist for many workers who need to take medical leave or have disabilities.
Ability to work and income security
The need for medical leave arises from a condition affecting workers’ own health and ability to perform their job duties. From an economic standpoint, this need itself can often pose a direct threat to individuals’ abilities to continue working and earning wages to support themselves and their families. In addition, the need to take medical leave often is unanticipated and unable to be planned.
As a result, many workers who need medical leave face an urgent threat to their economic stability. This is especially true for low-wage workers and even middle-income workers with little or no savings. Research shows that 41 percent of families do not have enough emergency funding to cover an unexpected $2,000 expense.9 For these families, taking weeks of leave to address a health condition without wage replacement would be very difficult or even financially catastrophic.
Need for medical leave
Whether paid or unpaid, all workers face the possibility of needing to take medical leave. The data on leave-taking under the Family and Medical Leave Act shows that it is the most commonly used type of leave. According to a survey by Abt Associates for the U.S. Department of Labor, 55 percent of all Family and Medical Leave Act claims were for medical leave, and it was the most common type of leave among both men and women.10 But, as we discussed earlier, access to paid medical leave varies by occupation, part-time status, and ethnicity.11 There are substantial unmet needs.12
While many workers need medical leave, the data show that it is used far less frequently than sick leave, with usage varying only somewhat by age and other factors. According to the National Health Interview Survey, a nationally representative survey, 35.1 percent of workers took 1 day to 5 days off work due to illness or injury, while only 10.6 percent of workers took 6 or more days off work in 2018.13 Over the period 1997 to 2018, the percent of employed individuals who reported taking no sick or medical leave ranged from 50 percent to 60 percent and varied little by age. The percentage of workers ages 45 and older who reported taking 6 or more days of leave was slightly higher than for those under age 45—10.4 percent compared to 8.1 percent, respectively.
Workers with less education and lower incomes reported relatively more days of leave. Meanwhile, far fewer workers leave the workforce entirely due to long-term disability. In 2018, approximately 4.1 percent of eligible workers received Social Security Disability Insurance.14
Private market for short-term disability insurance
In response to the broad need for medical leave, many employers provide sick and medical leave on a voluntary basis as part of their overall benefits and compensation packages. Some firms self-insure for these benefits or purchase group short-term disability insurance or use a third party to administer self-insured benefits. As a result, a large private insurance market exists for paid medical leave. In 2018, this market was estimated to have generated roughly $8.6 billion in premiums and covered 32.5 million individuals.15 Many of these insurers also offer long-term disability insurance, which generated premiums of roughly $18 billion in 2018 and covered more than 49.2 million individuals.
The existence of this private market has implications both for research and policy. The provision of private benefits could provide sources of variation that could be studied. In addition, private claims data may present opportunities for research, though proprietary interests may also impede this.
Policymakers also must consider the role of private insurance in public programs. Most state programs allow employers the ability to self-insure or provide benefits through a private plan, provided that the benefits are at least as generous as the state benefits (or better in some cases). Take-up of this option has been low so far, but as a growing number of states enact paid medical leave laws, more firms, including many large, multistate employers, may seek to provide a uniform set of benefits to all of their workers across the states through use of an opt-out mechanism. Federal policymakers will also need to consider this issue as they formulate proposals to cover all workers.
Return-to-work services
In addition to the wage replacement a worker receives while on medical leave, many employers with private plans also offer supportive services to their workers who face more challenging conditions or circumstances and may need additional assistance to return to work and stay at work. While most workers will be able to return to their jobs without additional help, others will face difficulties as they learn to navigate their postleave condition and its impact on their ability to function across each of the domains of their lives, including work, social, and personal environments.
Evidence-based return-to-work services focus on improving communication and coordination across these domains and intervening as early as possible after the onset of a new condition. Some workers, for example, may not know they are entitled to request reasonable accommodations when returning to work or may need help navigating the healthcare system, especially if they have multiple conditions being treated by more than one doctor. Return-to-work services can help workers understand their rights to accommodation.
Return-to-work services can be effective at improving health and employment outcomes and increasing worker retention by firms. In the United States, these services are largely provided on a voluntary basis by employers, so access is uneven and the quality of programs varies. In Europe and other developed countries, these services are more readily available because they are sometimes mandated alongside the provision of paid medical leave benefits. To date, these services in the United States have not been widely incorporated into individual state paid medical leave programs by state policymakers. But these services could play an important role in supporting positive health and employment outcomes for workers in publicly financed paid leave programs in the future.
Right to take medical leave and job protection
Paid medical leave policies do not exist in a vacuum. The Family and Medical Leave Act, Americans with Disabilities Act, Pregnancy Discrimination Act, and various state laws all affect workers’ rights to take job-protected leave. Lack of job protection can prevent workers from taking the leave they need. Under the Families and Medical Leave Act, workers at firms with 50 or more employees in a 75-mile radius are entitled to 12 weeks of unpaid, job-protected leave for parental, caregiving, and medical leave. To be eligible, the worker must have worked 1,250 hours for their employer over the past 12 months. In addition to the rights provided under the FMLA for all types of leave, individuals with work-limiting disabilities are also entitled to certain rights for leave-taking and benefits under the Americans with Disabilities Act, the Pregnancy Discrimination Act, and certain state laws.16
The Americans with Disabilities Act entitles employees with work-limiting disabilities to request medical leave and other forms of reasonable accommodation if they work for an employer with 15 or more employees. There is no length of service requirement. An employer, however, can refuse to grant an accommodation if it would impose undue hardship on the business. In contrast, employers covered by the Family and Medical Leave Act cannot refuse to grant leave due to hardship concerns, with exceptions for certain highly paid employees.17
Pregnant workers also are covered by the Pregnancy Discrimination Act, which provides protections on the basis of pregnancy, childbirth, or related medical conditions. Under this law, employers must treat pregnant workers in the same manner that they treat other temporarily disabled workers.18
Importantly, the federal Equal Employment Opportunity Commission issued a resource document in 2016 clarifying that workers with short-term medical conditions have a right to take medical leave as a form of reasonable accommodation from their employer under the Americans with Disabilities Act.19 This right applies to workers whether or not they are covered by the Family and Medical Leave Act, a state paid leave program, or an employer’s benefit plan—even if an employee exhausts other benefits. Yet a health condition must be substantially limiting for a worker to have medical leave rights under the Americans with Disabilities Act.
The Equal Employment Opportunity Commission cites examples such as a routine broken leg or hernia as conditions that generally would not qualify.20 For access to medical leave to be an accommodation, the leave must eventually enable the individual to return to work. That right includes job-protected time off from work and either paid or unpaid leave depending on an employer’s compensation package. In other words, the Americans with Disabilities Act effectively extends job protection to more workers taking medical leave than is available to workers taking parental or caregiving leave. As a result, workers who exhaust their paid or unpaid medical leave benefits could be entitled to additional leave before returning to work.
The Equal Employment Opportunity Commission resource document details that some workers taking medical leave may already have additional job protections and expanded access to benefits than workers taking parental or caregiving leave under the Family and Medical Leave Act. This is because both the Americans with Disabilities Act and the Pregnancy Discrimination Act apply to more employers and require no waiting period. Yet it is not clear how well understood this is by workers and to what extent workers on medical leave, who may not view themselves as having a disability, are exercising their rights.
With greater attention and advocacy, these stronger job protections and expanded access to benefits may influence the take-up rate of medical leave benefits by workers, particularly among low-wage workers. These factors could, in turn, greatly affect expected health and economic outcomes and have implications for the design of state and federal programs. Each of these areas warrant additional research.
Economic and health outcomes
A medical condition that requires workers to take time off from their jobs can entail risks to the health and economic well-being of those workers and their families. In the next two sections, we explore the literature around income security, disability, sick leave, and health more generally to understand how paid medical leave could affect economic and health outcomes when individuals experience a work-limiting medical condition.
Economic outcomes
As has become abundantly clear amid the current coronavirus recession, serious medical conditions that require time away from work can pose a threat to workers’ economic well-being. They can lead to an immediate reduction in income from wages while the worker is on leave, an increase in out-of-pocket expenses for medical care, and a heightened risk of job loss. Employers and the broader economy are also affected when work-limiting medical conditions lead to worker absences, reductions in productivity, and the loss of skilled staff. Government programs and spending are impacted as well when workers lose wages and employment and must turn to public assistance programs for support.
Paid medical leave could help address all of these challenges, but existing research on the direct of effects of paid medical leave specifically is scant and limited to specific medical conditions. Yet related research on sick leave, income security, occupational health, and disability programs suggests that paid medical leave could affect economic outcomes by reducing income volatility, helping workers to return to employment after taking leave, reducing productivity loses due to presenteeism, and supporting greater labor supply and long-term labor force participation.
Income volatility
Work-limiting medical conditions that threaten a worker’s economic stability often arise suddenly. These health and income shocks can put many medium- and low-wage workers and their families at risk of hardship when a medical condition forces someone to stop working for a period of time. A 2015 study by The Pew Charitable Trusts found that 1 in 3 families report having no savings at all, and that approximately 41 percent of families did not have enough emergency funding to cover an unexpected $2,000 expense.21 For these families, taking weeks of leave to address a health condition without wage replacement would be very difficult or even catastrophic.
A median worker’s weekly earnings in the third quarter of 2019 was $360, according to the U.S. Department of Labor’s Bureau of Labor Statistics.22 For this median wage worker, 12 weeks of unpaid medical leave would reduce gross take home pay by $4,320. And income disruptions, such as medical conditions requiring leave from work, are common. One study found that roughly 1 in 4 families experiences an income disruption in a year and that 5.1 percent of families experience an income disruption due to a health-related work limitation. These disruptions make families significantly more likely to face eviction and to miss payments for housing and utilities.23 Families dependent on a single wage earner are especially vulnerable.
Research on savings and assets, however, shows that even small amounts of savings can help families weather income disruptions. While 21.1 percent of families with savings of $249 or less missed a housing payment, that percentage falls to 15.2 percent when families have savings of between $250 and $749.24 Similarly, the additional income available to workers through paid medical leave could boost family finances enough to improve their ability to weather health-related income disruptions.
For many workers, a loss of wages due to medical leave is often further compounded by an increase in out-of-pocket medical expenditures—an important factor in analyzing the potential consequences for workers and families. A study of the 2007–2008 panel of the Medical Expenditure Panel Study, a 2-year longitudinal survey that builds upon the National Health Interview Survey, found workers with a temporary disability pay approximately 22 percent of their healthcare expenditures out of pocket, or an average of $388.25 More broadly, the Federal Reserve found that “one-fifth of adults had major, unexpected medical bills to pay.” These bills most often totaled between $1,000 and $4,999, and about 40 percent of those with bills had unpaid debt.26
A Journal of the American Medical Association research letter summarized a survey of patients with stage III colorectal cancer that found respondents without paid sick or medical leave reported significantly higher personal financial burden, including a higher rate of borrowing money and having difficulty making credit card payments, and a significantly greater likelihood of leaving their job.27 In addition, workers who lose their jobs may also lose access to employer-provided health insurance.
Older workers may also be at greater risk of economic hardship as a result of experiencing a serious medical condition. One study compiled 20 years of data from the Health and Retirement Study, a nationally representative panel survey of the elderly and near-elderly, and examined a 10-year panel of credit reports for adults in California with hospital admissions. The study found that in the 3 years after a hospitalization, older workers saw earnings decline by 19 percent —similar to the earnings decline associated with a job displacement. For these older workers, higher out-of-pocket medical expenditures posed a hardship, but the loss of earnings was three times larger.28
There is also evidence that wage insurance for workers who acquire long-term disabilities can improve financial security for those awarded benefits compared to those who were denied. A study of Social Security Disability Insurance benefits using variations in benefit awards based on age-related eligibility rules found that after workers were awarded benefits, they faced substantially lower risks of bankruptcy, home foreclosure, and eviction.29
Employment outcomes and return to work supports
In addition to providing wage replacement and job protections to workers, some employer-provided short-term disability benefits also include services for workers who need additional help returning to work following a new illness or injury or the worsening of a chronic condition. A large body of research exists on the effectiveness of return-to-work programs and suggests that they play an important role in improving workers’ employment rates, earnings levels, and worker retention rates for employers. Below, we summarize major findings from studies inside and outside the United States, including workplace-based and healthcare-facilitated programs.
A number of systematic reviews have been done summarizing the evidence on employer-provided return-to-work interventions. Some of the evidence on these programs comes from the United States, but more research has been done on programs outside the country, where return-to-work services are more widespread and usually provided as part of employers’ mandated responsibilities to employees experiencing work-limiting medical conditions.
Overall, the literature suggests that the most effective programs emphasize early intervention following the onset of a new condition or worsening of a chronic condition. Below, we highlight key findings in more detail.
- One review found that effective early-intervention programs that address multiple domains of a worker’s life, including the workplace, healthcare, and personal/social environments, were the most effective at increasing the likelihood of a person returning to work.30
- Two reviews found that evidence-based, early-intervention programs had a significant positive impact on the likelihood of workers with common mental disorders returning to work.31
- Three reviews found that early intervention programs that addressed multiple domains were effective at shortening the duration of work absence following the onset of a range of new potentially disabling conditions, including musculoskeletal, pain-related, and mental health conditions.32 Evidence was mixed on the effectiveness of interventions that only addressed one domain.33
Other studies also have looked at the benefits to employers from return-to-work programs. A survey of large California employers found that those with established disability management or return-to-work programs retained workers who developed work-based impairments at a significantly greater rate and that injured workers returned to work 1.4 times faster than a comparable group.34 Similarly, another study found workers who received workplace accommodations from their employer were 40 percent more likely to continue working, though the impact faded over time.35 And a study by the Integrated Benefits Institute found that employees who worked for employers with formal return-to-work programs had shorter leave durations than those without formal programs.36 More research is needed, however, to better understand which U.S.-based employer programs are effective and how those could inform policy.
Evidence from healthcare-based approaches
While return-to-work services are primarily provided through employer-based disability management programs, there are some examples in the United States of other approaches. These models use government funding to provide return-to-work services through a worker’s connection to a state or community healthcare system. Two primary examples include the Washington State Centers for Occupational Health and Education, which primarily addresses musculoskeletal conditions that arise from occupational injuries, and the more widespread Individual Placement and Support model, which assists people with serious mental illness.
The Washington State Centers for Occupational Health and Education is part of Washington state’s worker’s compensation program and assists workers who have work-related illnesses and injuries and need additional support to return to work. This program’s model emphasizes early intervention and improved communication between the injured worker, the physician’s office, and the employer. An 8-year follow-up evaluation of the program found that, relative to a comparable group of injured workers, workers receiving this state intervention had a 30 percent reduction in workplace-based disability and 30 percent lower rate of injured workers transitioning to Social Security Disability Insurance.37
Another study found that the Washington State Centers for Occupational Health and Education’s approach helped detect and address excess prescriptions of opioids.38 A recent randomized controlled trial in the United Kingdom tested practices similar to those used by the Washington state program. The authors found a reduction in days off work and improved performance at work, for a substantial net estimated return on investment.39 The Washington state program’s model is used to assist workers with a wide array of conditions, but the largest focus is on assisting workers with musculoskeletal conditions, which are among the most common types of conditions underlying workers’ compensation claims, as well as disability and medical leave generally.
Another model for assisting individuals with severe mental illness is the Individual Placement and Support model. Under this model, an employment specialist is placed within the medical treatment team, and services can be delivered through community mental health centers. When a client expresses an interest in employment, the specialist provides job-placement assistance and continued support while the person is working. This model is based on eight principles that include honoring client preferences, initiating a job search as soon as a person is interested, and integrating the employment services with mental health treatment services.
There are an extensive set of Individual Placement and Support studies in the United States and abroad, including at least 21 randomized controlled trials. Overall, experts conclude that Individual Placement and Support is the most effective model for supporting employment for people with mental illness. Studies have found it is effective in increasing employment rates, but more data is needed to determine whether there is a lasting long-term effect on employment from the intervention.40
Understanding how return-to-work services could be provided effectively in connection with paid medical leave requires more research. Rhode Island has taken a step in this direction by introducing a partial return-to-work benefit for workers who return to work on a part-time basis. A study of the data from that state used to administer the short-term disability benefit concluded the data could be useful for targeting return-to-work services to the highest risk workers.41 Similarly, a study of the California short-term disability benefit and worker’s compensation programs identified ways in which the two programs could help target at-risk workers for services and found opportunities to collect better data to improve the accuracy and timeliness of services.42
Employee productivity
From the research, it is not yet clear whether expanded paid medical leave increases or decreases overall productivity. Studies in this area focus on how productivity declines when employees continue working while they are sick, a behavior known as presenteeism. A substantial body of research in the United States and abroad is expanding our understanding of the extent of presenteeism. Some research narrowly focuses on measuring the amount of work that occurs when a worker should have taken sick or medical leave. Other research takes a broader approach and looks at all types of poor health. As not all types of health problems require long leaves, some research on presenteeism also considers the cost of episodic and chronic conditions, such as allergies, arthritis, and gastrointestinal disorders, among others.
This body of evidence finds that presenteeism imposes significant costs on employers. Workers who continue working while ill are often less productive. In other words, the net cost to employers of workers taking medical leave should be measured compared to the diminished productivity of a worker who would otherwise be working while ill. A study of the total economic impact to employers resulting from chronic health conditions concluded that the cost of presenteeism “greatly exceeded the combined cost of absenteeism and medical treatment.”43
Another study focused on the 10 most common health conditions and compiled data from surveys and an employer absence-management database, and found the cost of presenteeism represented the majority of employer costs for most of the conditions—higher than medical costs and ranging from 18 percent to 60 percent for all the conditions.44 There is anecdotal evidence that major employers are recognizing these costs and developing programs to reduce the cost of presenteeism.45 In addition, a structured systematic review found “presenteeism costs are rarely included in full economic evaluations.”46
The relative amount of productivity loss from presenteeism is difficult to estimate, and it is especially difficult to isolate the productivity loss for those workers who would otherwise have taken paid medical leave if it was available. A study using the RAND American Life Panel, a nationally representative, internet-based survey, concluded that overall, nearly two-thirds of the U.S. workforce reports working while sick in the past year, with productivity losses averaging around 20 percent.47
The prevalence of presenteeism means that the analysis of the costs and benefits associated with expanding access to medical leave must consider how increased costs from additional leave-taking may be partially or fully offset by reduced costs from presenteeism and improved health. A study of a change in Swedish medical leave policy to eliminate the waiting period and increase benefit generosity, for example, resulted in an increase in short spells of leave and a decrease in long spells, for an overall reduction in absenteeism.48 We have not identified any research that has attempted to estimate the net change in productivity from an expansion of paid medical leave.
Labor force participation and implications for other government programs
Creating a new paid medical leave benefit could have implications for long-term U.S. labor force participation and other government programs, in particular Social Security Disability Insurance. Yet the nature of the relationship between a such a benefit and labor supply is complex and not fully understood.
In the short term, access to paid medical leave may reduce the risk of job separations. One study using several panels of the Medical Expenditure Panel Study, which provides a 2-year longitudinal follow-up to the National Health Interview Survey, found that access to paid sick leave reduced job separations, suggesting paid medical leave may have a similar effect. More specifically, the study found that, after controlling for many worker and job characteristics, “paid sick leave decreases the probability of job separation by at least 2.5 percentage points, or 25 percent.”49 This effect is comparable to what has been found with employer-provided health insurance. In addition, some experts suggest that a medical leave or short-term disability benefit creates an opportunity for employers to provide supports and accommodations that could improve overall labor force participation.50
Over the longer term, some research suggests that the provision of short-term disability benefits, which are typically offered for a duration of 6 months or longer, can increase applications to long-term disability insurance by reducing the costs associated with the long waiting period for those benefits.51 But studies are mixed on the extent to which this moral hazard exists.52
In addition, it is not clear whether or how these findings pertain to paid medical leave benefits that are shorter in duration, such as those that only last 12 weeks. One study that looked at a change in German law to reduce the generosity of benefits for sick leaves lasting longer than 6 weeks found no evidence that the duration of absences decreased, as would be expected if a significant moral hazard existed.53 Yet this study also found that lower-income and middle-aged subgroups may be more sensitive to these changes. Similarly, one study used the gradual phase-in of nine city-level and four state-level sick leave pay mandates on employers and found neither employment nor wage growth was significantly affected.54
Return-to-work services also can affect labor supply and costs to other programs. Research on the Washington State Centers for Occupational Health and Education intervention discussed earlier found that for each worker this intervention helped to avoid Social Security Disability Insurance, it helped an additional two workers avoid long-term work disability and unemployment without government assistance.55 Another study using worker’s compensation data estimated that injured workers who were provided workplace accommodations—one component of many return-to-work interventions—delayed their Social Security Disability Insurance applications by 4.4 years on average.56
Paid medical leave benefits also have important implications for other government programs beyond Social Security Disability Insurance. The onset of poor health is a significant factor in early withdrawals of savings from 401(k) retirement plans.57 Paid medical leave could help workers avoid or reduce the extent to which they tap retirement savings to deal with health shocks. For lower-income workers eligible for means-tested programs, such as the Supplemental Nutrition Assistance Program, taking unpaid medical leave could increase their food stamp benefits.
Using National Health Interview Survey data and controlling for many factors, one study found that working-age adults without paid sick leave are 1.41 times more likely to receive income from a state or county welfare program and 1.34 times more likely to receive Supplemental Nutrition Assistance Program benefits.58 Workers who receive paid leave benefits also contribute additional tax revenue based on those benefits. Similarly, to the extent that paid medical leave supports labor force participation, it also leads to higher contributions to the Social Security trust funds, both strengthening the financing of these programs overall and increasing a worker’s retirement benefits.
Health outcomes
Research on the impact of paid medical leave on health outcomes is still emerging. Evidence to date suggests there are several different mechanisms through which paid medical leave may have an effect. These include improved health management, earlier treatment, greater healthcare utilization, improved income stability, reduced financial stress, and enhanced return-to-work supports. In this section, we discuss what current research says about how these potential pathways could impact individual health, public health, and healthcare spending and how it can inform future work.
Better health management
One of the strongest signals that paid medical leave may impact health outcomes comes from research on paid sick leave. Broadly speaking, having access to paid sick leave is associated with a significantly lower risk of mortality across a wide range of conditions.59 The nature of this relationship is still being studied, but evidence suggests access to paid sick leave better enables workers to manage a new health condition, for instance, by seeking preventative care and earlier treatment of conditions.
Data from the National Health Interview Survey appears to support this idea. One study found that workers with access to paid sick leave were significantly more likely to seek preventive medical care, such as mammograms, pap tests, and endoscopies than other workers after controlling for other factors.60 Studies also have found that when workers have access to sick leave, they take more time off work for health-related reasons.61 These workers also visit the emergency room less.62 These findings suggest that workers with paid leave may be better able to schedule medical appointments, thereby avoiding the use of emergency rooms for less-urgent conditions.
Conversely, workers without access to paid sick leave are significantly less likely to receive preventive health screenings, even when they are aware that they face higher medical risks.63 These findings also are important because early treatment of a health condition has been found to reduce the severity and duration of the condition.64
Delaying or forgoing leave while sick or injured can have serious health consequences. One longitudinal study of a cohort of civil servants in the United Kingdom, known as the Whitehall II study, found that unhealthy men who took no sick leave were twice as likely to experience a serious coronary event compared to unhealthy men who took moderate amounts of sick leave.65 Similarly, a study that linked responses to a survey of Danish workers with administrative data on social welfare payments found that respondents who went to work ill more than six times over the past year had a 53 percent higher risk of taking medical leave for at least 2 weeks, and a 74 percent higher risk of taking leave for more than 2 months after adjusting for confounding factors.66
But not all the evidence is clear or consistent. A doctoral dissertation using the Medical Expenditure Panel Survey did not find clear patterns of a change in leave-taking when workers experienced a job change that makes them lose or gain access to paid sick leave.67
Public health
The literature on paid sick leave suggests paid time off to address certain illnesses may have important positive effects on public health by helping to reduce the spread of contagious diseases. This evidence could have implications for medical leave or show opportunities for new research. An analysis of local and state sick leave mandates in the United States using Google Flu Trend data found a significant reduction in the general flu rate after the mandates were implemented.68 These public health benefits also have spillover benefits for employers through reduced absenteeism.
One study using seven panels of Medical Expenditure Panel Survey data concluded that paid sick leave reduces overall absenteeism by reducing the spread of influenza-like illness. They estimated that reduced absenteeism due to paid sick leave could have saved employers $0.63 billion to $1.88 billion per year in 2016 dollars.69 It is possible that paid medical leave that extends beyond a few days or a couple of weeks could also impact public health, but to what extent is unclear since many conditions that require longer-duration leaves may not be contagious.
At a minimum, the experience with the coronavirus pandemic and the incidences of contracting COVID-19 is demonstrating the need for longer leaves to help individuals recover from the illness itself and to quarantine to protect others and stop the spread of the new coronavirus. This time is in addition to what is needed to care for family members who may be sick, quarantined, or home due to school or work closures.
Reducing negative health effects from stress
Paid medical leave may also improve health outcomes for workers by reducing stress associated with a financial insecurity due to a health shock. As we explored in the previous section of this report, taking time away from work to address a medical condition is a common source of financial strain for workers and families, one that can also add stress on workers who are already concerned with their health. Stress, regardless of its source, has been shown to negatively impact physical and mental health.70 In addition, research from developed countries shows that income levels directly affect mortality.71 Severe debt also is correlated with poor health.72
To the extent that paid medical leave reduces stress associated with financial strain, it could also lead to improved health for workers. Research on the impact of the Earned Income Tax Credit, which provides income to lower-paid workers, including many without any federal tax liabilities, and disability benefits suggests income supports can have significant positive effects. A study of the impact of an increase in the Earned Income Tax Credit in 1993 was associated with an improvement in maternal health. It is thought that a reduction in financial stress was an important factor.73
Similarly, a study taking advantage of the discontinuities in the Social Security Disability Insurance benefit formula finds “that $1,000 in annual payments decreases the annual mortality rate of lower-income beneficiaries by approximately 0.1 to 0.25 percentage points.” The same study also finds that beneficiaries with higher past earnings and the largest disability benefits did not experience the same benefits.74
Supporting workers after illness and injury
In the earlier section on economic outcomes, we discussed the role of return-to-work services in supporting positive economic outcomes for workers who take paid medical leave. Research on evidence-based, return-to-work interventions shows that they can also impact worker’s health. Much of the research focuses on quantifying these effects in terms of the duration of leave and savings to employers from reduced short-term disability claims and lower healthcare expenditures.
Examples of how return-to-work interventions affect health and employers’ costs come from the United States and other developed countries. We first summarize studies that primarily address musculoskeletal conditions. In the United States, an evaluation of the Washington State Centers for Occupational Health and Education program discussed earlier showed that workers who received the intervention had 19.7 percent fewer days off work and a reduction in total disability and medical costs of $510 per claim.75 A randomized control trial in Finland also found that the ability to take leave intermittently can be important. The study found that when workers were provided with intermittent leave instead of full-time leave, recovery times were significantly shorter.76
Another set of studies found that return-to-work interventions can be effective in assisting workers with depression. One systematic review of these interventions found evidence suggesting the approaches that combined different therapeutic interventions showed the most promise in reducing depression levels among workers. But they also cautioned that many of the studies included in the review were small and that more research is needed.77
An extensive review funded by the U.S. Department of Health and Human Services of the literature on work-focused interventions for depression compiled by Westat Corp, which provides research services to the federal government, identified the Be Well At Work model, a work-based depression-counseling intervention conducted through a series of telephone sessions, as the most promising U.S.-based program. Two controlled trials of Be Well At Work found that the intervention reduced depression and absenteeism and improved work performance. But there have not been any evaluations of the model under real-world conditions, so more testing is needed.78
Overall healthcare spending
To the extent that access to paid medical leave could improve worker health, it could also lead to cost savings if those improvements reduce disability leave durations and overall healthcare spending. Analysis using the Truven (now IBM) Health MarketScan research databases, which includes a large amount of data on employees covered by private disability insurance, suggests that longer disability leaves are moderately correlated with higher health expenditures.79 They found that a third of the most expensive cases overall were also among the longest in duration.
The study also found that musculoskeletal conditions are the top driver of medical costs and disability durations, but that lengthy, intensive medical treatment was not always related to length of leave. They concluded that healthcare and return-to-work interventions will be more effective if they take into account psychosocial and other barriers to disability.
Another analysis using the same data source found that a quarter of all workers in the survey took a temporary leave following an illness or injury.80 These workers were associated with approximately 60 percent of total healthcare and disability payments. They estimated that the total economic impact of employee illness, including losses in productivity from disability leaves, was approximately $6.5 billion over the period of 2008–2012.
Remaining questions and opportunities for research
Research on paid sick and medical leave, disability, occupational health, and income security programs suggests that paid medical leave could have significant positive impacts on economic and health outcomes for individuals and employers, as well as implications for our society and the U.S. economy more broadly. There are, however, important gaps in our understanding of paid medical leave, and future research could help address those gaps in a number of ways.
Collect more data and analyses of how workers use paid and unpaid medical leave
These needed data and analyses include the duration of leaves, types of conditions, and the recovery and return-to-work rates. In addition, understanding how workers use paid and unpaid leave varies by gender, race, and other socioeconomic variables, the better understanding of which would inform policy development.
Understand better the use of unpaid medical leave
Getting a better bead on the use of unpaid medical leave is particularly important among low-wage workers with the least access. But also important to understand is how unpaid leave affects economic outcomes, including measures of financial security such as eviction, bankruptcy, debt levels, and access to credit. Could ameliorating health and financial shocks help workers and families? Could it contribute to enhanced economic mobility? How does job protection affect these outcomes?
Conduct more research on how access to paid medical leave affects health outcomes
There is evidence that the availability of paid medical leave increased leave-taking and use of medical services, thereby potentially speeding recovery and return to work. But there are many questions that need to be answered to understand this effect more thoroughly. Among those questions:
- Does more leave and more healthcare usage equal better health, and for whom?
- How are the effects similar to or different from paid sick leave? How does the availability of longer leaves affect health and recovery?
- Does it vary by type of condition?
- What is the impact, for example, of leave for pregnancy-related conditions on mothers and infants?
- Could paid medical leave affect public health?
The recent outbreak of COVID-19 suggests medical leave could be important for treatment and containment of contagious diseases requiring longer leaves. What can be learned from recently enacted legislation to support workers dealing with COVID-19 is another new and important line of inquiry.
Conduct more research to understand better how sick leave and medical leave policies interact
Paid sick leave is usually now provided through employers while paid medical leave can be provided by either employers or government agencies. Where benefits are provided through multiple sources, research is needed on which approach and duration of benefits best address the needs of ill and injured workers.
Conduct more research on U.S.-based return-to-work services
There is evidence that well-designed return-to-work services for at-risk workers can improve employment and health outcomes, yet much of the research is in an international context and interventions are usually workplace or healthcare-based. Future research could help us understand which interventions are most promising in the U.S. context, which can be scaled up effectively in the country, and which can be provided to workers through the connection with public paid medical leave benefits. Also in need of further research is the role return-to-work services should play in supporting positive health and economic outcomes from paid medical leave.
Better understand how medical leave benefits vary across public and private plans
Employers have a longstanding role in the provision of paid medical leave, especially for higher-paid workers. But employers have mixed incentives in providing these benefits that are at odds with the interests of workers. A government agency has a more neutral role but is not directly involved in the employment relationship.
More research could be done to understand how outcomes vary under private versus public benefits, including how access to benefits and effective return-to-work services vary under each model.
Better understand paid leave programmatic designs
Future research could inform programmatic design questions. How should public programs use private medical guidelines in the review of claims and appeals? Can these sources be helpful in identifying at-risk workers who would benefit from return-to-work services? How can access and usage of leave be expanded among low-wage and vulnerable populations?
Better understand health and economic inequalities in all their dimensions
Across all the areas discussed above, more research is needed to understand the impact of paid medical leave along key socioeconomic dimensions, including income level, age, race, and gender. This point is being driven home today by the starkly uneven consequences of the coronavirus pandemic and resulting recession on those members of our society and their families already experiencing the legacies of inequality stretching back generations, particularly African American workers and their family members.81
Conclusion
Paid medical leave helps workers addresses serious medical conditions that require time away from work. The need for medical leave is often difficult to predict and can threaten a person’s well-being and livelihood. And while many workers will only need shorter-term sick leave over the course of their career, others may face multiple health challenges.
There is comparatively less research on the direct effects of paid medical leave on health and economic outcomes relative to parental and family caregiving leave. But related research suggests the social insurance protections provided by paid medical leave can have many benefits for workers and their families by enabling workers to better manage their health condition, return to work quickly, and prevent negative consequences from the stress and financial shock associated with a new work-limiting medical condition. Workers may take more leave, but the absenteeism effect may be offset by reductions in periods of low productivity from presenteeism.
A well-designed paid medical leave program that supports better health and stronger connections to work also can also benefit the broader economy and reduce government spending on other income security and healthcare programs. Future research on paid medical leave could help to build the evidence base by demonstrating causal links between policy and outcomes. It could also help deepen our understanding of each of the pathways through which paid medical leave can affect workers, employers, the U.S. economy, and public health.
Further work in this area is important and salient, heightened most recently by the COVID-19 crisis. Public awareness of the need for paid sick and medical leave and the substantial gaps in availability of these benefits is increasingly clear. With enactment of the Families First Coronavirus Response Act, the first federal legislation that provides emergency paid sick and caregiving leave to workers, policymakers must now consider whether and how to pursue long-term policy in these areas.
About the authors
Jack Smalligan is a senior policy fellow in the Income and Benefits Policy Center at the Urban Institute. He analyzes the interactions across disability, retirement, and paid leave policy. Previously, he was deputy associate director at the Office of Management and Budget, serving five administrations since 1990. In 2012, he was a visiting fellow at The Brookings Institution, where he analyzed the Social Security Disability Insurance program. Smalligan received a master’s degree in public policy from the University of Michigan.
Chantel Boyens is a principal policy associate in the Income and Benefits Policy Center at the Urban Institute. Her current work focuses on interactions between Social Security programs and retirement, pensions, disability, and paid leave policy. Before joining the Urban Institute, Boyens was acting branch chief and senior program examiner in the Income Maintenance Branch of the Office of Management and Budget for 9 years and across two administrations. Boyens received a master’s degree in public policy from American University.
Acknowledgments
This report was written with support from Arnold Ventures. The authors appreciate the helpful suggestions of Alix Gould-Werth, Sam Abbott, Jeff Hayes, and Molly Weston Williamson. We also want to thank the design and editorial team at the Washington Center for Equitable Growth—Dave Evans, Maria Monroe, Emilie Openchowski, and Ed Paisley—for their sharp editing, design, and web layout work.
Appendix: Data sources
Expanding the evidence base on medical leave entails some data challenges. One challenge is that surveys that ask workers the amount of leave they have taken for health-related reasons usually capture a combination of sick leave, medical leave, and short-term disability benefits. In addition, not all surveys indicate whether the leave was paid or unpaid. Another challenge is that it can be generally difficult to identify significant health impacts from policy changes, even from much larger changes as the Medicaid expansion under the Affordable Care Act.82 Despite these challenges, there are a number of important resources that could be used for future research.
Below, we discuss some of these resources and their potential applications for future research. This summary builds on the broader framework laid out in “Paid Family and Medical Leave in the United States: A Data Agenda.”83 We begin by identifying several surveys frequently used in medical leave research, then describe a variety of longitudinal surveys that offer research opportunities, and conclude by identifying other surveys most frequently used for all types of paid leave research.
The National Health Interview Survey, conducted by the National Center for Health Statistics, annually measures the amount of health-related leave taken and whether the leave was paid or unpaid.
The Medical Expenditure Panel Survey builds upon the National Health Interview Survey data and is conducted by the Agency for Healthcare Research and Quality, with five interviews over a 2.5-year period using respondents from the original interview. This survey also collects data on paid and unpaid leave.
The Panel Study of Income Dynamics, conducted by the University of Michigan, collects data on sick and medical leave, including the frequency with which a worker has needed to take 3 or more weeks of leave. While this panel study has a much longer follow-up period than the Medical Expenditure Panel Survey, it doesn’t measure whether workers have access to paid leave.
The Health and Retirement Study, undertaken through a cooperative agreement between the National Institute on Aging and the University of Michigan, is a national longitudinal survey that provides resources for medical leave research for subsets of individuals. It asks participants the number of days they missed work because of their health and whether they earn paid sick leave.84 While this survey is limited to individuals ages 50 and older, it provides for a longer longitudinal panel than the Medical Expenditure Panel Survey and has not been used as extensively as the National Health Interview Survey and Medical Expenditure Panel Survey to analyze sick and medical leave.
The National Health and Aging Trend Study, conducted by the Johns Hopkins University Bloomberg School of Public Health in collaboration with the University of Michigan, has data on sick and medical leave but is only focused on individuals who are over the age of 65.85
The American Time Use Survey, conducted by the Bureau of Labor Statistics, provides the most detailed data on use of paid and unpaid leave at a single point in time, though leave data is only available periodically.86 The Leave and Job Flexibilities Module for this survey covering 2017 to 2018 provides richer data than the overall annual survey and is financed by the U.S. Department of Labor’s Women’s Bureau.87
The Family and Medical Leave Act Survey, conducted by Abt Associates with funding by the U.S. Department of Labor, periodically surveys employers and employees on use of leave covered by the Family and Medical Leave Act, with the last report covering 2012. This survey does not always differentiate the amount of leave taken for specific unpaid leave purposes, such as medical leave. The most recent survey was administered from August 2016 until August 2019, and the results have not yet been released.
Additional sources with some data include the Annual Social and Economic Supplement to the Current Population Survey and the Survey of Income and Program Participation, both conducted by the Census Bureau, and show up less frequently in the literature.88
The American Working Conditions Survey, part of the RAND American Life Panel conducted by the RAND Corporation, uses a nationally representative internet panel and a 3-year follow-up, and has data on health-related work absences, including paid and unpaid sick leave and working while sick.
The Commonwealth Fund Biennial Health Insurance Survey, a national survey of Americans ages 19 to 64 conducted by the Commonwealth Fund, asks about health-related leave but does not distinguish between own medical leave and leave to care for an ill family member.
Data on the number of workers with access to formal paid sick and temporary disability leave benefits is most readily available from the U.S. Bureau of Labor Statistics National Compensation Survey of employers. The International Foundation of Employee Benefit Plans also surveys employers and publishes data on the characteristics of private benefits.89 Both these data sources are useful to understand how many workers are covered by formal plans, but cannot shed light on the amount employees use of the benefits. Also, it is important to compare the coverage rates as shown in the National Compensation Survey with use of paid leave as reported by workers in the Family and Medical Leave Act survey and the American Time Use Survey.90
States that already provide paid leave benefits are another source of data. For the longstanding state programs (California, New Jersey, New York, and Rhode Island), paid leave was added to existing temporary disability programs. These programs provided disability benefits more comparable to private short-term disability insurance—benefit durations of 26 weeks or more. Washington state now has a program providing 12 weeks of paid medical leave that began issuing benefits this year and will be an important source of data in the future. In addition, the District of Columbia will begin paying benefits this year, followed by Massachusetts, Connecticut, and Oregon over the next 3 years. As Amy Batchelor, from the Office of Management and Budget, notes, linking this state data with Unemployment Insurance earnings data or the U.S. Census Bureau’s Longitudinal Employer-Household Dynamics program has great potential.91
With employers funding much of the medical leave provided in the United States, some of the richest administrative data exists in privately held databases. This data has been analyzed primarily to improve the provision of employer-provided benefits and has been rarely used to better understand a publicly provided medical leave benefit. One of the largest and most frequently cited private databases is the IBM MarketScan® Research Databases (formerly Truven MarketScan). One study uses this to chart absence rates and consider the correlation between duration of absence and magnitude of health expenditures. The Integrated Benefits Institute is another resource. It has assembled data for the IBI Benchmarking Analytics tool that pools 6 million claims from 15 disability insurers and 65,000 employer policies.92
While likely not a resource for academic research, it is worth noting that in the United States, there are two large, proprietary databases that provide recommended leave durations based on medical conditions and other factors. These databases are used by private companies and some state governments when reviewing medical leave and disability claims. These guidelines, which include MDGuidelines and ODG (originally titled Official Disability Guidelines), tap many sources, including expert opinion and academic research, as well as thousands and sometimes millions of leave-usage reports from employers and intermediaries. Leave-duration recommendations are based on the nature of a worker’s job requirements, age, gender, and co-morbidities, such as obesity. But exactly how these factors are used to formulate recommendations is not fully understood. The existence of these databases raises a question of whether and how they might be used in the context of federal proposals to establish a national paid medical leave program.
End Notes
1. Bureau of Labor Statistics, Employee Benefits in the United States—March 2019 (U.S. Department of Labor, 2019), table 16: Insurance benefits: Access, participation, and take-up rates, private industry workers, March 2019.
2. National Partnership for Women and Families, “State Paid Family and Medical Leave Insurance Laws” (2019).
3. Hawaii also operates a temporary disability insurance program. For more information, see “About Temporary Disability Insurance,” available at https://labor.hawaii.gov/dcd/home/about-tdi/ (last accessed April 26, 2020).
4. National Partnership for Women and Families, “Paid Sick Days—State and District Statuses” (2019).
5. Bureau of Labor Statistics, Employee Benefits in the United States—March 2019.
6. Bureau of Labor Statistics, “Economic News Release: Access to and Use of Leave, Table 7: Workers who needed to take leave from their jobs but did not take it: reasons for needing to take leave by selected characteristics, averages for the period 2017-2018,” Press release, August 29, 2019, available at https://www.bls.gov/news.release/leave.t07.htm.
7. Occupational illnesses and injuries are addressed through workers’ compensation programs and fall outside the scope of this paper. For more information, see “Workers’ Compensation,” available at https://www.dol.gov/general/topic/workcomp (last accessed April 26, 2020).
8. Molly W. Williamson, “The Meaning of Leave: Understanding Workplace Leave Rights,” N.Y.U. Journal of Legislation and Public Policy 22 (2019): 197–268.
9. The Pew Charitable Trusts, “The Role of Emergency Savings in Family Financial Security: What Resources do Families Have for Financial Emergencies?” (2015).
10. Jacob Alex Klerman, Kelly Daley, and Alyssa Pozniak, “Family Medical Leave in 2012: Technical Report” (Cambridge, MA: Abt Associates, 2012).
11. Ann P. Bartel and others, “Racial and ethnic disparities in access to and use of paid family and medical leave: evidence from four nationally representative datasets” (Washington: Bureau of Labor Statistics, 2019).
12. Bureau of Labor Statistics, “Economic News Release: Access to and Use of Leave, Table 7: Workers who needed to take leave from their jobs but did not take it: reasons for needing to take leave by selected characteristics, averages for the period 2017-2018.”
13. Authors’ calculations.
14. Social Security Administration, The 2019 OASDI Trustees Report (2019), table V.C5—DI Beneficiaries With Benefits in Current-Payment Status at the End of Calendar Years 1975-2095.
15. National Association of Insurance Commissioners, “2018 Accident and Health Policy Report Experience Report” (2019).
16. Many states have job protection laws for medical leave in addition to the federal laws, sometimes as part of a paid medical leave benefit program.
17. Under the FMLA, and subject to strict requirements, employers may sometimes refuse to restore certain highly paid employees to their prior position under what is known as the “key employee” exception. For more information, see “Family and Medical Leave Act Advisor,” available at https://webapps.dol.gov/elaws/whd/fmla/9e4.aspx (last accessed April 26, 2020).
18. U.S. Equal Employment Opportunity Commission, “Fact Sheet: Pregnancy Discrimination” (1997), available at https://www.eeoc.gov/eeoc/publications/fs-preg.cfm.
19. U.S. Equal Employment Opportunity Commission, “Employer-Provided Leave and the Americans with Disabilities Act” (2016), available at https://www.eeoc.gov/eeoc/publications/ada-leave.cfm.
20. U.S. Equal Employment Opportunity Commission, “The Family and Medical Leave Act, the Americans with Disabilities Act, and Title VII of the Civil Rights Act of 1964” (1995), available at https://www.eeoc.gov/policy/docs/fmlaada.html.
21. The Pew Charitable Trusts, “The Role of Emergency Savings in Family Financial Security: What Resources do Families Have for Financial Emergencies?”
22. Bureau of Labor Statistics, “Economic News Release: Usual Weekly Earnings of Wage and Salary Workers, Table 1: Median usual weekly earnings of full-time wage and salary workers by sex, quarterly averages, seasonally adjusted,” Press release, January 17, 2020, available at https://www.bls.gov/news.release/wkyeng.t01.htm.
23. Signe-Mary McKernan and others, “Thriving Residents, Thriving Cities: Family Financial Security Matters for Cities” (Washington: Urban Institute, 2016). Note: Income disruptions were defined as either an involuntary job loss, onset of a health-related work limitation, or a drop in family income of at least 50 percent.
24. Ibid.
25. Chaiporn Pumkam and others, “Health care expenditures among working-age adults with physical disabilities: Variations by disability spans,” Disability and Health Journal 6 (4) (2012): 287–296.
26. Board of Governors of the Federal Reserve System, “Report on the Economic Well-Being of U.S. Households in 2018” (2019).
27. Christin M Veenstra and others, “Association of Paid Sick Leave With Job Retention and Financial Burden Among Working Patients With Colorectal Cancer,” JAMA 314 (24) (2015): 2688–2690.
28. Carlos Dobkin and others, “The Economic Consequences of Hospital Admissions,” American Economic Review 108 (2) (2018): 308–352.
29. Ibid; Manasi Deshpande, Tal Gross, and Yalun Su, “Disability and distress: The effect of disability programs on financial outcomes.” Working Paper (Washington Center for Equitable Growth, 2019).
30. Andrea Gragnano and others, “Common Psychosocial Factors Predicting Return to Work After Common Mental Disorders, Cardiovascular Diseases, and Cancers: A Review of Reviews Supporting a Cross-Disease Approach,” Journal of Occupational Rehabilitation 28 (2) (2018): 215–31.
31. Mai Bjornskov Mikkelsen and Michael Rosholm, “Systematic Review and Meta-Analysis of Interventions Aimed at Enhancing Return to Work for Sick-Listed Workers with Common Mental Disorders, Stress-Related Disorders, Somatoform Disorders and Personality Disorders,” Journal of Occupational and Environmental Medicine 75 (9) (2018): 675–86; Sabdh Joyce and others, “Workplace Interventions for Common Mental Disorders: A Systematic MetaReview,” Psychological Medicine 46 (4) (2016): 683–97.
32. K.L. Cullen and others, “Effectiveness of Workplace Interventions in Return-to-Work for Musculoskeletal, Pain-Related and Mental Health Conditions: An Update of the Evidence and Messages for Practitioners,” Journal of Occupational Rehabilitation 28 (1) (2018): 1–15; William Johnson and others, “Disability Risk Management and Post Injury Employment of Workers with Back Pain,” Risk Management and Insurance Review 15 (1) (2012): 35–55; Renée-Louise Franche and others, “Workplace-Based Return-to-Work Interventions—A Systematic Review of the Quantitative Literature,” Journal of Occupational Rehabilitation 15 (4) (2005): 607–31.
33. K.L Cullen and others, “Effectiveness of Workplace Interventions in Return-to-Work for Musculoskeletal, Pain-Related and Mental Health Conditions: An Update of the Evidence and Messages for Practitioners.”
34. Christopher McLaren, Robert Reville, and Seth Seabury, “How Effective Are Employer Return to Work Programs?” Working Paper WR-745-CHSWC (RAND Corporation, 2010).
35. Matthew Hill, Nicole Maestas, and Kathleen Mullen, “Employer Accommodation and Labor Supply of Disabled Workers,” Labor Economics 41 (2016): 291–303.
36. Brian Gifford and Skyler Parry, “The Value of Disability Return-to Work Programs” (San Francisco, CA: Integrated Benefits Institute, 2016).
37. Thomas Wickizer, Gary Franklin, and Deborah Fulton-Kehoe, “Innovations in Occupational Health Care Delivery Can Prevent Entry into Permanent Disability: 8-year Follow Up of the Washington State Centers for Occupational Health and Education,” Medical Care 56 (12) (2018): 1018–23.
38. Gary Franklin and others, “A Comprehensive Approach to Address the Prescription Opioid Epidemic in Washington State: Milestones and Lessons Learned,” American Journal of Public Health 105 (3) (2015): 463–69.
39. Gwenllian Wynne-Jones and others, “Effectiveness and Costs of a Vocational Advice Service to Improve Work Outcomes in Patients with MSK Pain in Primary Care: A Cluster Randomized Trial,” Pain 159 (2018): 128–38.
40. Bonnie O’Day and others, “Preventing Unemployment and Disability Benefit Receipt among People with Mental Illness: Evidence Review and Policy Significance,” Psychiatric Rehabilitation Journal 40 (2) (2017): 123–52; Tina Marshall and others, “Supported Employment: Assessing the Evidence,” Psychiatric Services 65 (1) (2014): 16–23; Alison Luciano, Gary Bond, and Robert Drake, “Does Employment Alter the Course and Outcome of Schizophrenia and Other Severe Mental Illnesses? A Systematic Review of Longitudinal Research,” Schizophrenia Research 159 (2–3) (2014): 312–321; Julia Baller and others, “Long-Term Follow-Up of the Mental Health Treatment Study.” Paper presented at the 5th Annual Meeting of the Social Security Disability Research Consortium in Washington (2017); Judith A. Cook, Jane K. Burke-Miller, and Emily Roessel, “Long-Term Effects of Evidence-Based Supported Employment on Earnings and on SSI and SSDI Participation Among Individuals with Psychiatric Disabilities,” American Journal of Psychiatry 173 (10) (2016): 1007–14.
41. Annette Bourbonniere and David Mann, “Benefit Duration and Return to Work Outcomes in Short Term Disability Insurance Programs: Evidence from Temporary Disability Insurance Program,” Journal of Occupational Rehabilitation 28 (4) (2018): 597–609.
42. Frank Neuhauser, Yonaton Ben-Shalom, and David Stapleton, “Early Identification of Potential SSDI Entrants in California: The Predictive Value of State Disability Insurance and Workers’ Compensation Claims,” Journal of Occupational Rehabilitation 28 (2018): 574–583.
43. James Collins and others, “The Assessment of Chronic Health Conditions on Work Performance, Absence, and Total Economic Impact for Employers,” Journal of Occupational and Environmental Medicine 47 (6) (2005): 547–557.
44. Ron Z. Goetzel and others, “Health, Absence, Disability, and Presenteeism Cost Estimates of Certain Physical and Mental Health Conditions Affecting U.S. Employers,” Journal of Occupational and Environmental Medicine 46 (4) (2004): 398–412.
45. Paul Hemp, “Presenteeism: At Work—But Out of It,” Harvard Business Review 82 (10) (2004): 49–58.
46. Jesse Kigozi and others, “The Estimation and Inclusion of Presenteeism Costs in Applied Economic Evaluation: A Systematic Review,” Value in Health 20 (3) (2017): 496–506.
47. Nicole Maestas, Kathleen J. Mullen, and Stephanie Rennane, “Absenteeism and Presenteeism Among American Workers.” Paper presented at 6th Annual Meeting of the Disability Research Consortium in Washington (2018).
48. Per Pettersson-Lidbom and Peter Skogman Thoursie, “Temporary Disability Insurance and Labor Supply: Evidence from a Natural Experiment,” Scandinavian Journal of Economics 115 (2) (2013): 485–507.
49. Heather Hill, “Paid Sick Leave and Job Stability,” Work and Occupations 40 (2) (2013): 143–173.
50. David Autor and Mark Duggan, “Supporting Work: A Proposal for Modernizing the U.S. Disability Insurance System” (Washington: Center for American Progress and The Hamilton Project, 2010).
51. Michael Stepner, “The Long-Term Externalities of Short-Term Disability Insurance.” Working Paper (2019), available at http://economics.mit.edu/grad/stepner/research.
52. David H. Autor and others, “How does Access to Short Term Disability Insurance Impact SSDI Claiming?” Paper No. NB 13-09 (NBER Disability Research Center, 2013); David Autor, Mark Duggan, and Jonathan Gruber, “Moral Hazard and Claims Deterrence in Private Disability Insurance.” Working Paper No. 18172 (NBER, 2012); Elisabeth Fevang, Ines Hardoy, and Knut Røed, “Temporary Disability and Economic Incentives,” The Economic Journal 127 (603) (2017): 1410–1432; Pettersson-Lidbom and Skogman Thoursie, “Temporary Disability Insurance and Labor Supply: Evidence from a Natural Experiment.”
53. Nicolas R Ziebarth, “Long-Term Absenteeism and Moral Hazard—Evidence from a Natural Experiment,” Labour Economics 24 (2013): 277–292.
54. Stefan Pichler and Nicolas R. Ziebarth, “Labor Market Effects of U.S. Sick Pay Mandates,” Journal of Human Resources (forthcoming).
55. Thomas Wickizer, Gary Franklin, and Deborah Fulton-Kehoe, “Innovations in Occupational Health Care Delivery Can Prevent Entry into Permanent Disability: 8-year Follow Up of the Washington State Centers for Occupational Health and Education,” Medical Care 56 (12) (2018): 1018–23.
56. Richard Burkhauser, J.S. Butler, and Robert R Weathers II, “How Policy Variables Influence the Timing of Applications for Social Security Disability Insurance,” Social Security Bulletin 64 (1) (2001): 52–83.
57. Teresa Ghilarducci and others, “Household Economic Shocks Increase Retirement Wealth Inequality” (New York: The Schwartz Center for Economic Policy Analysis, 2016).
58. Patricia Stoddard-Dare and others, “Paid sick leave status in relation to government sponsored welfare utilization,” American Journal of Orthopsychiatry 88 (5) (2018): 608–615.
59. Daniel Kim, “Paid Sick Leave and Risks of All-Cause and Cause-Specific Mortality among Adult Workers in the USA,” International Journal of Environmental Research and Public Health 14 (10) (2017): 1247.
60. Lucy A. Peipins and others, “The lack of paid sick leave as a barrier to cancer screening and medical care-seeking: results from the National Health Interview Survey,” BMC Public Health (2012).
61. Thomas Ahn and Aaron Yelowitz, “Paid Sick Leave and Absenteeism: The First Evidence from the U.S,” SSRN Electronic Journal (2016); Maestas, Mullen, and Rennane, “Absenteeism and Presenteeism Among American Workers”; David M. Zimmer, “Employment Effects of Health Shocks: The Role of Fringe Benefits,” Bulletin of Economic Research 67 (4) (2015): 346–358.
62. Kevin Miller, Claudia Williams, and Youngmin Yi, “Paid Sick Days and Health: Cost Savings from Reduced Emergency Department Visits” (Washington: Institute for Women’s Policy Research, 2011).
63. LeaAnne DeRigne and others, “Paid sick leave and preventive health care service use among U.S. working adults,” Preventive Medicine 99 (2017): 58–62.
64. Mark Murray and Donald M. Berwick, “Advanced Access: Reducing Waiting and Delays in Primary Care,” JAMA 289 (8) (2003): 1035–1040; Julia C. Prentice and Steven D. Pizer, “Delayed Access to Health Care and Mortality” Health Services Research 42 (2) (2007): 644–662.
65. Mika Kivimäki and others, “Working While Ill as a Risk Factor for Serious Coronary Events: The Whitehall II Study,” American Journal of Public Health 95 (1) (2005): 98–102.
66. C.D. Hansen and J.H .Andersen, “Sick at work—a risk factor for long-term sickness absence at a later date?” Journal of Epidemiology and Community Health 63 (5) (2009): 397–402.
67. Ryan Spencer Klein, “Evaluating Health and Healthcare Use Effects of Changes in Paid Sick Leave Access for Workers in the United States,” Ph.D. dissertation, University of Minnesota, 2016, available at http://hdl.handle.net/11299/183355.
68. Stefan Pichler and Nicolas Ziebarth, “The Pros and Cons of Sick Pay Schemes: Testing for Contagious Presenteeism and Noncontagious Absenteeism Behavior,” Journal of Public Economics 156 (2017): 14–33.
69. Abay Asfaw, Roger Rosa, and Regina Pana-Cryan, “Potential Economic Benefits of Paid Sick Leave in Reducing Absenteeism Related to the Spread of Influenza-Like Illness,” Journal of Occupational and Environmental Medicine 59 (9) (2017): 822–829.
70. Peggy Thoits, “Stress and Health: Major Findings and Policy Implications,” Journal of Health and Social Behavior 51 (S) (2010): S41–S53.
71. David M. Cutler, Angus S. Deaton, and Adriana Lleras-Muney, “The Determinants of Mortality” Journal of Economic Perspectives 20 (3) (2006): 97–120.
72. Thomas Richardson, Peter Elliot, and Ronald Roberts, “The relationship between personal unsecured debt and mental and physical health: A systematic review and meta-analysis,” Clinical Psychology Review 33 (8) (2013): 1148–1162.
73. William N. Evans and Craig L. Garthwaite, “Giving Mom a Break: The Impact of Higher EITC Payments on Maternal Health,” American Economic Journal: Economic Policy 6 (2) (2014): 258–290.
74. Alexander Gelber, Timothy Moore, and Alexander Strand, “Disability Insurance income saves lives.” Working Paper 18-005 (Stanford Institute for Economic Policy Research and NBER, 2018).
75. Thomas Wickizer and others, “Improving quality, preventing disability and reducing costs in workers’ compensation healthcare: A population-based intervention study,” Medical Care 49 (12) (2011): 1105–1111.
76. Eira Viikari-Juntura and others, “Return to work after early part-time sick leave due to musculoskeletal disorders: a randomized controlled trial,” Scandinavian Journal of Work, Environment and Health 38 (2) (2012): 134–43.
77. Wan Yunus and others, “Systematic Review of Universal and Targeted Workplace Interventions for Depression,” Occupational and Environmental Medicine 75 (1) (2018): 66–75.
78. Gary R. Bond and others, “Work Focused Interventions for Depression” (Rockville, MD: Westat, 2019).
79. Catherine Zaidel and others, “Health Care Expenditures and Length of Disability Across Medical Conditions,” Journal of Occupational and Environmental Medicine 60 (7) (2018): 631–636.
80. Brian Gifford, “Temporarily Disabled Workers Account for a Disproportionate Share of Health Care Payments,” Health Affairs 36 (2) (2017): 245–249.
81. Alex Bäcker, “Why COVID-19 May Be Disproportionately Killing African Americans: Black Overrepresentation among COVID-19 Mortality Increases with Lower Irradiance, Where Ethnicity Is More Predictive of COVID-19 Infection and Mortality Than Median Income” (2020), available at https://ssrn.com/abstract=3571699.
82. Tyler N.A. Winkelman and Virginia W. Chang, “Medicaid Expansion, Mental Health and Access to Care Among Childless Adults with and without Chronic Conditions,” Journal of General Internal Medicine 33 (3) (2018): 376–383.
83. Amy Batchelor, “Paid Family and Medical Leave in the United States: A Data Agenda” (Washington: Washington Center for Equitable Growth, 2019), available at https://equitablegrowth.org/research-paper/paid-family-and-medical-leave-in-the-united-states-2/?longform=true#paid_medical_leave.
84. “The Health and Retirement Study,” available at https://hrs.isr.umich.edu/about (last accessed March 2, 2020).
85. NHATS at a Glance,” available at https://www.nhats.org/ (last accessed March 2, 2020).
86. Bureau of Labor Statistics, “Economic News Release: Access to and Use of Leave, Table 6. Workers who took leave from their jobs during an average week, hours of leave taken, and type of leave used, by main reason for taking leave, averages for the period 2017-2018,” Press release, August 29, 2019, available at https://www.bls.gov/news.release/leave.t07.htm.
87. Bureau of Labor Statistics, “Access to and Use of Leave Summary,” Press release, August 29, 2019, available at https://www.bls.gov/news.release/leave.nr0.htm.
88. Ann P. Bartel and others, “Racial and ethnic disparities in access to and use of paid family and medical leave: evidence from four nationally representative datasets.”
89. International Foundation of Employee Benefit Plans, “Employee Benefits Survey: 2018 Survey Results” (2019).
90. Isabel V. Sawhill, Sarah Nzau, and Katherine Guyot, “A primer on access to and use of paid family leave” (Washington: Brookings Institution, 2019).
91. Batchelor, “Paid Family and Medical Leave in the United States: A Data Agenda”; “Longitudinal Employer-Household Dynamics,” available at https://lehd.ces.census.gov/ (last accessed March 2, 2020).
92. Benchmarking,” available at https://www.ibiweb.org/benchmarking/ (last accessed March 2, 2020).